Incidental findings on ultrasonography suggest that 20- 60% of the general population has thyroid nodules.4 Though most thyroid nodules do not produce symptoms and are rarely cancerous, some can grow very large and produce excess hormones that cause discomfort in your body. Whether or not you require treatment depends on your symptoms’ severity and can be determined by your primary care physician. Today, we will go over some traditional and novel treatment options that your doctor can offer depending on your type of thyroid nodule and symptoms.
Malignant Nodules
Malignant, or cancerous, nodules are treated quickly upon diagnosis to prevent the spread of cancer through the tissue, lymph nodes, or bloodstream. Approximately 5-15% of thyroid nodules are malignant.4
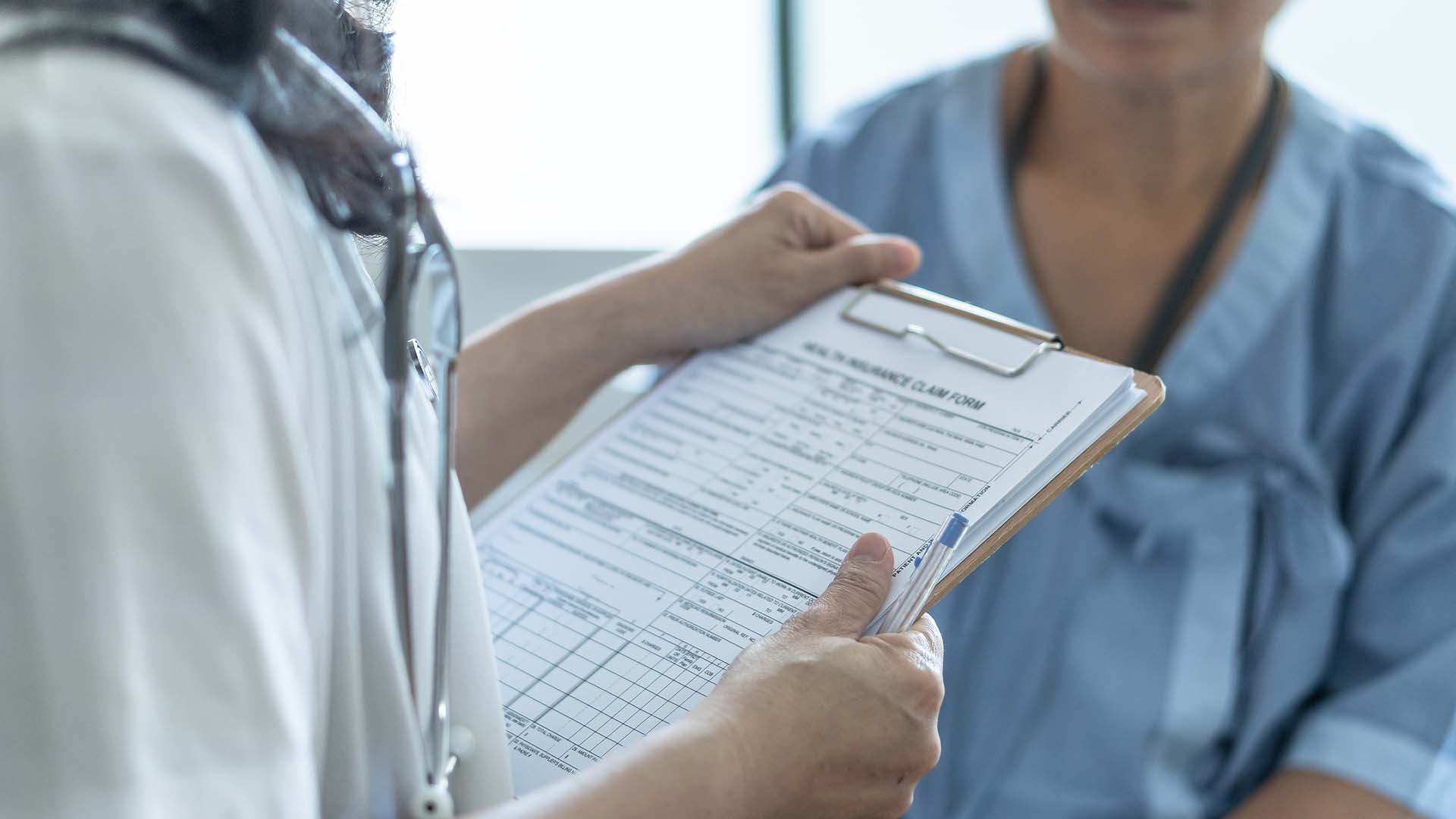
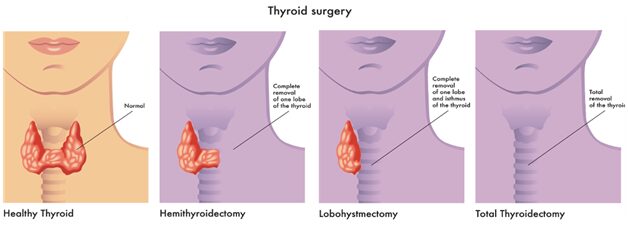
Surgery
At present, surgery is the most common treatment option for malignant nodules. You may undergo three common surgeries to remove malignant nodules: hemithyroidectomy, lobectomy, and total thyroidectomy.1
Radiation Therapy
Radiation therapy utilizes x-ray and other types of radiation to kill cells or prevent them from multiplying. Follicular and papillary thyroid cancers can be treated by radioactive iodine therapy (RAI). The iodine is mainly taken up by the thyroid cells, which destroys the thyroid gland and any thyroid cells (including cancerous and non-cancerous cells) that take up iodine while leaving the rest of the body unaffected.1
Benign Nodules
Benign nodules account for 85- 95% of all thyroid nodules. Other than cosmetic concerns, the most common indications for treating thyroid nodules include difficulty swallowing, shortness of breath, and other systemic symptoms caused by the overproduction of thyroid hormones.
Observation with Regular Follow Up
For most benign nodules, observation and regular follow-up is the primary form of treatment. This treatment option consists of regular monitoring of any changes in your thyroid nodules by your physician, either through physical examinations or ultrasound assessments. Thyroid nodules can proliferate quickly. In one study, the focus group’s thyroid nodules had a median increase in the size of 114% over 51 months. 3
Hormone Therapy
Hormone therapy is a preventative treatment option. This option consists of two parts. The first is blocking the stimulating thyroid hormone, and the second is taking thyroid hormone replacement pills in the case of underproduction of thyroid hormone. The combination of these two steps could help prevent cancer cells from growing.1
Percutaneous Ethanol Injection (PEI) for Cystic Nodules
Percutaneous Ethanol Injection, or PEI, is a treatment option that utilizes alcohol injection to reduce the nodules’ size and volume. This treatment is most commonly used to treat benign cystic (fluid-filled) thyroid lesions with an overall efficacy rate of 80-100%.2 This treatment option also offers a less than 5% chance of recurrence.2
Radiofrequency Ablation (RFA) for Solid Nodules
Radio Frequency Ablation (RFA) is a treatment option that uses thermal energy created by radiofrequency to ablate (burn) the nodules, reducing the size and volume of the benign lesion. This treatment is most commonly used to treat benign solid (tissue-filled) thyroid nodules. According to a study by Jeong et al., they observed an 85% reduction in nodular volume after 6-months post-treatment.5 Over 80% of the patients achieved over 58% nodule shrinkage within one-month post-treatment.
Microwave (MWA) / Laser Ablation (LA)
Microwave and laser ablation treat thyroid nodules using thermal energy generated by microwave and laser energy, respectively.
According to a recent study by Shi et al., both procedures have a very similar volume reduction rate, with laser ablation achieved slightly superior performance. On average, both approaches achieved around 60% and 64% volume reduction within 3- and 6-months post-treatment, respectively.4 By 12 months, both procedures were observed to reduce the nodular volume by approximately 81%.4
Speak to a specialist today to explore your treatment options.